If you’ve been looking for a good reason to slim down, consider this: Being obese at midlife appears to increase your odds for dementia.
That’s the takeaway from a large study just published by British researchers, and it echoes similar findings published in December.
Dorina Cadar, lead researcher on the new study, said the goal is to identify risk factors that are influenced by lifestyle so steps can be taken to prevent mental decline.
A Secret Weapon For Weight-Loss and Management!
“We hope that a substantial portion, but admittedly not all, of dementia cases can be prevented through public health interventions,” she said. Cadar is a senior research fellow at University College London.
Obesity and Dementia Findings
Her team found that people who are obese at midlife have a 31% higher risk for dementia than middle-aged people whose weight is normal – and the risk is especially high for women.
The good news: Losing weight may significantly lower the odds, the researchers said.
For the study, Cadar and her colleagues analyzed data from nearly 6,600 people aged 50 and older who were part of a British study on aging. The researchers used three sources to ascertain dementia: doctor diagnosis, informant reports and hospital statistics.
While obesity was a risk for both men and women, the risk of dementia was even higher for women with abdominal obesity – a condition measured by their waist size. Over an average follow-up of 11 years, they were 39% more likely to develop dementia, the study found.
This higher risk was independent of other factors, such as age, education, marital status, smoking, genetics, diabetes and high blood pressure. No association between abdominal obesity and dementia was found among men, the study authors said.
But when the researchers considered both weight and waist size together, obese men and women alike had 28% higher odds of developing dementia.
A study published in December of women only uncovered similar risks. Dr. Sam Gandy, associate director of the Mount Sinai Alzheimer’s Disease Research Center in New York City, reviewed the new findings.
“This new paper is entirely consistent with both the field in general and with our own work in particular,” he said.
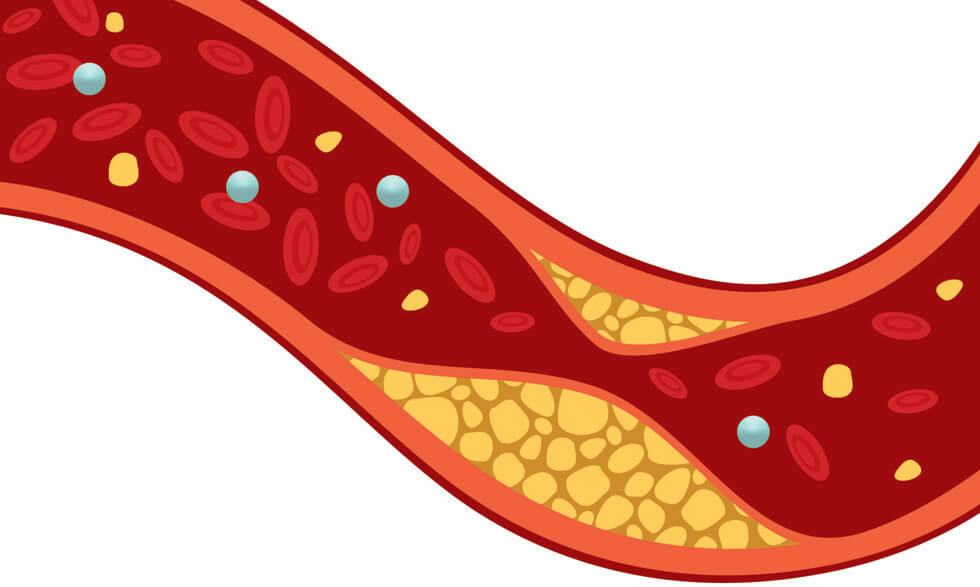
Gandy said proteins implicated in inflammation, cardiovascular disease and type 2 diabetes – all of which are risk factors for Alzheimer’s – may contribute to the links between obesity and
dementia.
Keith Fargo, director of scientific programs and outreach at the Alzheimer’s Association, said links between underlying causes of chronic physical conditions and dementia are well known.
“The association between heart health risk factors – such as diabetes, obesity and high blood pressure – and cognitive decline and dementia is well established in Alzheimer’s research,” Fargo said.
These new findings add to the overall body of evidence that links obesity to higher dementia risk, he noted. The sex-based differences identified in the latest study are intriguing, Fargo said.
The Alzheimer’s Association is running a two-year clinical trial to see if healthy lifestyle interventions that target risk factors can protect cognitive function in a diverse group of older adults.
What is really interesting is the strong evidence that living more healthfully can reduce dementia risk.